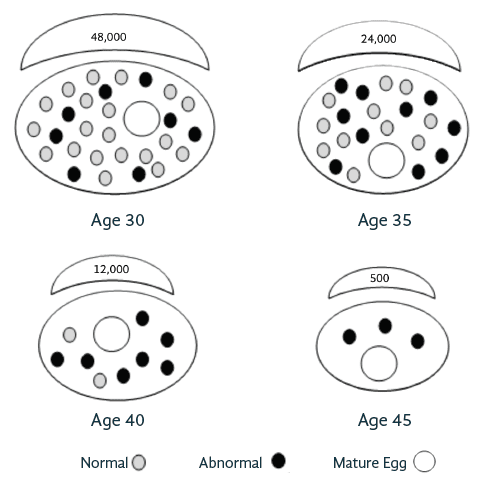
This chart illustrates the likelihood of pregnancy per month when actively trying to conceive based on age. It also explains the rise in miscarriage rates as we get older because of the increased number of abnormal eggs, the primary reason for miscarriages.
| AGE | 30 | 35 | 40 | >42 |
|---|---|---|---|---|
| % Pregnancy/month | 15 - 20% | 10 - 15% | 5 - 8% | 4% |
| % Miscarriage | 15 - 20% | 20 - 25% | 30 - 40% | >50% |
| % Genetically Abnormal Embryos | 25 - 30% | 40 - 60% | 70 - 80% | >80% |
These pictorial ovals demonstrate an ovary and shows how an ovary at age 30 is much larger than an ovary at age 45. It also highlights how the total number of eggs decrease with age and the total number of abnormal eggs increase with age. The dots represent the follicles that can be seen on ultrasound, the half-shaped moon represents the overall egg supply that cannot be seen on ultrasound.
Follicles seen on ultrasound reflect a small fraction of the residual pool.
*Note, this illustration is an average. The absolute number and quality of eggs diminishes with age, but the number of follicles is variable for everyone. A younger person may have a lower number of antral follicles but the quality is still good versus an older person with a higher number of eggs but poor egg quality.
Reproductive aging is the main predictors of whether or not one will be able to conceive. There is an expected natural decline in fertility with advanced aging. The rate of this decline, however, cannot be predicted for a given individual.
If you and a partner have been attempting pregnancy for >6 months (if age 35 or older) or >12 months (younger than 35) we recommend scheduling a New Patient Visit at SRM for a full fertility workup.
